|
|
A hormone to break the obesity cycle?
While obesity rates for pregnant women continue to climb, scientists have discovered they can increase a specific hormone during pregnancy and reduce, or possibly, eliminate the chances the babies born will become obese as well.
Obese pregnant women often give birth to babies at risk for diabetes. "In the U.S., nearly two-thirds of women enter pregnancy either overweight or obese," explains study senior author Thomas Jansson, MD, PhD a professor at the University of Colorado Anschutz Medical Campus. "That makes them susceptible to gestational diabetes, preterm labor and preeclampsia. At the same time, the baby is often born larger with more fat than normal."
These infants often become obese adults too, setting up a vicious cycle that drives the obesity epidemic. So Jansson and his research team set out to break the cycle. They focused on the hormone Adiponectin which makes people sensitive to insulin.
High levels of Adiponectin guard against obesity and diabetes — low levels put people at risk.
Adiponectin acts as a brake to the amount of nutrients passed through the placenta of a pregnant woman. Low levels of adiponectin allow more nutrients to flow through, resulting in a larger than normal baby with more body fat.
Scientists tested the affects of Adiponectin by infusing it into obese and pregnant mice during the last four days of their normal 20-day gestational period — about equal to the last trimester of human pregnancy. The increase normalized the hormone balance in the mom mice.
"It completely reversed all the negative effects on the placenta. The pups of the obese mice had completely normal weights. Their glucose levels were also normal. We were able to pre-empt all the usual negative consequences of these kinds of pregnancies. This hormone or a similar agent could feasibly do the same thing for humans that it did for mice."
Thomas Jansson, MD, PhD a professor at the University of Colorado Anschutz Medical Campus
More work needs to be done to track the long-term effects of this hormone treatment over the life of a mouse, "But we have laid the foundation for what we believe might ultimately help break the cycle of obesity that has approached epidemic proportions in our society," Jansson adds.
Another group of researchers have developed a compound similar to Adiponectin that can be taken orally, and are now in clinical trials.
This study is published in the Proceedings of the National Academy of Sciences or PNAS.
Significance
Obesity and metabolic syndrome may, in part, originate in fetal life. In particular, babies of mothers with obesity and/or gestational diabetes mellitus (GDM) are often large at birth and have increased adiposity, which predisposes them to the development of metabolic disease later in life. Maternal obesity and GDM are typically associated with low circulating levels of adiponectin (ADN), and we found that ADN supplementation to pregnant obese mice completely normalized the changes in placental function and prevented fetal overgrowth caused by maternal obesity. These findings suggest that strategies to increase ADN levels in maternal obesity and GDM may alleviate the adverse effects of these pregnancy complications on the fetus.
Abstract
Mothers with obesity or gestational diabetes mellitus have low circulating levels of adiponectin (ADN) and frequently deliver large babies with increased fat mass, who are susceptible to perinatal complications and to development of metabolic syndrome later in life. It is currently unknown if the inverse correlation between maternal ADN and fetal growth reflects a cause-and-effect relationship. We tested the hypothesis that ADN supplementation in obese pregnant dams improves maternal insulin sensitivity, restores normal placental insulin/mechanistic target of rapamycin complex 1 (mTORC1) signaling and nutrient transport, and prevents fetal overgrowth. Compared with dams on a control diet, female C57BL/6J mice fed an obesogenic diet before mating and throughout gestation had increased fasting serum leptin, insulin, and C-peptide, and reduced high-molecular-weight ADN at embryonic day (E) 18.5. Placental insulin and mTORC1 signaling was activated, peroxisome proliferator-activated receptor-α (PPARα) phosphorylation was reduced, placental transport of glucose and amino acids in vivo was increased, and fetal weights were 29% higher in obese dams. Maternal ADN infusion in obese dams from E14.5 to E18.5 normalized maternal insulin sensitivity, placental insulin/mTORC1 and PPARα signaling, nutrient transport, and fetal growth without affecting maternal fat mass. Using a mouse model with striking similarities to obese pregnant women, we demonstrate that ADN functions as an endocrine link between maternal adipose tissue and fetal growth by regulating placental function. Importantly, maternal ADN supplementation reversed the adverse effects of maternal obesity on placental function and fetal growth. Improving maternal ADN levels may serve as an effective intervention strategy to prevent fetal overgrowth caused by maternal obesity.
The study was published Monday in the Proceedings of the National Academy of Sciences. The co-authors include, Fredrick J. Rosario, PhD, instructor at CU Anschutz, Professor Theresa Powell, PhD, of CU Anschutz and Irving L. M. Aye of Cambridge University in England.
Return to top of page
|
|
|
Oct 1, 2015 Fetal Timeline Maternal Timeline News News Archive
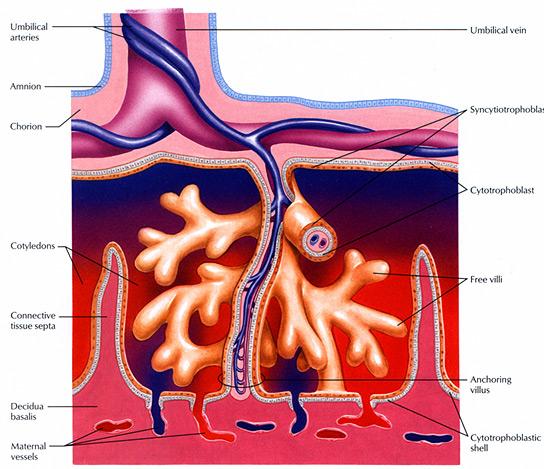
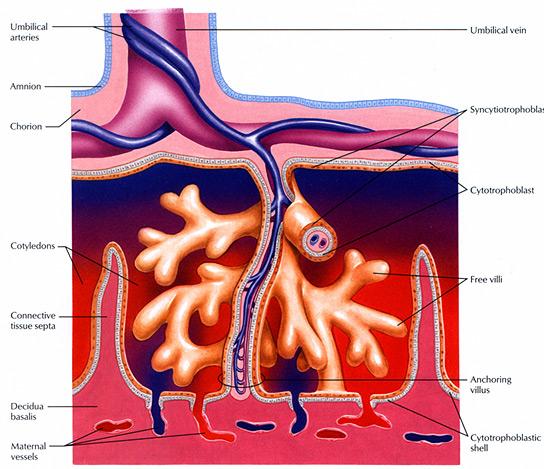
The placental blood system regulates molecular substances between mother and fetus.
Adiponectin acts as a brake to the amount of nutrients passing through the placenta.
Image Credit: Wright State University
|
|
| |
|