|
|
Generating placental cells from skin cells.
Regenerative medicine is new and expanding and aims to replace lost or damaged cells, tissues and organs in the human body. Now, placental cells may be added to the list.
In 2006, two Japanese scientists, Nobel laureate Shinya Yamanaka and Kazutoshi Takahashi, showed, that introduction of four genes into skin cells can reprogram fibroblasts into functional embryonic stem-like cells (also called "induced pluripotent stem cells" ("iPSCs").
The notion that as few as four genes can completely change a cell, opened new avenues for scientists to attempt to convert different adult cells into other somatic cell types. Several subsets of cell types — blood cells, nerve cells, heart cells, liver cells — were created from different adult stem cells.
The discovery that iPSCs can be induced to become somatic cell types, opened an avenue to resolve both ethical concerns and immune rejection problems associated with ESCs as the source of donor cells.
Now, researchers from the Hebrew University of Jerusalem, led by Dr. Yosef Buganim in the Faculty of Medicine, Department of Developmental Biology and Cancer Research at the The Institute for Medical Research Israel-Canada (IMRIC), have succeeded in converting skin cells into stable and fully functional placenta-generating cells — also called induced trophoblast stem cells or iTSCs.
The placenta is the least understood human organ, but arguably one of the most important.
When the placenta does not develop properly or is damaged, recurrent miscarriage and other placental insufficiencies occur.
It influences the lifelong health of a woman and all of her children during each pregnancy.
Placental dysfunction diseases are associated with low birth weight, premature birth and birth defects. One potential outcome can be Fetal Growth Restriction or FGR. Also called Intrauterine Growth Restriction or IUGR, FGR tends towards mild mental retardation and in severe cases - fetal death. IUGR also carries increased risk of complications for the mother.
But to date, attempts to grow human placenta precursor cells in the lab have failed. Without a placental model system, research on origination of problems and subsequent treatment is limited.
In an attempt to generate full-function placenta-generating cells, Dr. Buganim and colleagues screened a mouse model for genes supporting placental development.
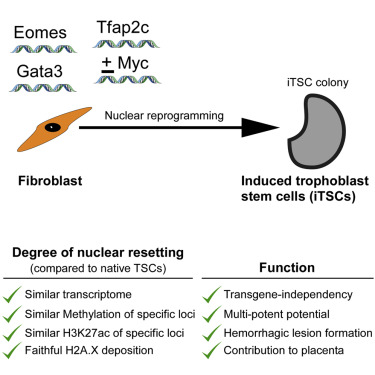
Researchers have identified three genes — Gata3, Eomes and Tfap2c — that when introduced into skin cells, completely convert them into stable and fully functional placenta-generating cells. These skin-derived TSCs look like natural TSCs, and function and contribute to the developing placenta.
The research paper is published in the journal Cell Stem Cell.
Now, the main focus of the Buganim lab is to generate fully functional human placenta-generating cells. Their success might grant a real chance to women who suffer from recurrent miscarriage and placental dysfunction to have healthy babies.
It is important to note that these cells do not hold any risk to the feus as they integrate only into the placenta and not into the embryo itself.
Abstract Highlights
•Gata3, Eomes, and Tfap2c expression convert cells into induced trophoblast stem cells
•Gata3, Eomes, Tfap2c, and Myc induce rapid mesenchymal-to-epithelial transition (MET)
•Induced trophoblast stem cells form hemorrhagic lesions and chimerized E13.5 placenta
•Induced trophoblast stem cells can be generated from Oct4 knockout MEFs
Summary
Induced pluripotent stem cells (iPSCs) undergo extensive nuclear reprogramming and are generally indistinguishable from embryonic stem cells (ESCs) in their functional capacity and transcriptome and DNA methylation profiles. However, direct conversion of cells from one lineage to another often yields incompletely reprogrammed, functionally compromised cells, raising the question of whether pluripotency is required to achieve a high degree of nuclear reprogramming. Here, we show that transient expression of Gata3, Eomes, and Tfap2c in mouse fibroblasts induces stable, transgene-independent trophoblast stem-like cells (iTSCs). iTSCs possess transcriptional profiles highly similar to blastocyst-derived TSCs, with comparable methylation and H3K27ac patterns and genome-wide H2A.X deposition. iTSCs generate trophoectodermal lineages upon differentiation, form hemorrhagic lesions, and contribute to developing placentas in chimera assays, indicating a high degree of nuclear reprogramming, with no evidence of passage through a transient pluripotent state. Together, these data demonstrate that extensive nuclear reprogramming can be achieved independently of pluripotency.
The Hebrew University of Jerusalem is Israel's leading academic and research institution, producing one-third of all civilian research in Israel. For more information, visit http://new.huji.ac.il/en.
Related article: Placenta on a chip
Return to top of page
|
|
|
Oct 16, 2015 Fetal Timeline Maternal Timeline News News Archive
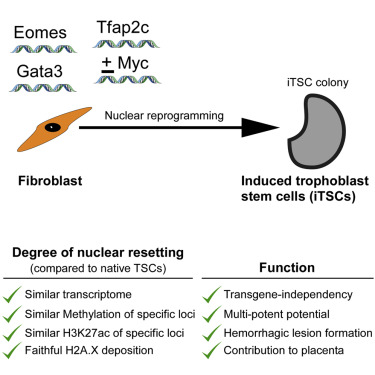
c-Myc is called "OSKM" or the "Yamanaka factor" for its role in transitioning
adult skin cells [fibroblasts] into other cell types such as placental cells —
also known as induced trophoblast stem cells, iTSCs.
Image Credit: Cell Stem Cell
|
|
| |
|